The Role of Hormones in Hunger and Fullness

It’s 4:00 PM. Not “time” for dinner yet. But your stomach is burning and growling so loud you think everyone around you can hear it. You know the feeling, but did you know that a hormone in your body is flooding messages to your brain that you need food? There are lots of hormones involved with the way our bodies recognize hunger and fullness, but the four main ones are Insulin, Cortisol, Ghrelin and Leptin. There’s also convincing studies that suggest the amount of sleep a person gets can alter how each of these hormones work. So, let’s get down to it, shall we?
What are Hormones?
I like to think of hormones as little messengers. They send and receive alerts between our body’s organs like the brain, thyroid, kidneys, pancreas, reproductive organs, heart, gut, placenta (for pregnant women), thymus, skin, and even fat tissues.
Insulin
Insulin is made in the pancreas and acts as a carrier for sugar. It carries sugar from the blood and brings it into cells to be used as energy. Think of it as the back hoe that takes dirt from the ground and dumps it into a dump truck for later use.
Long-term consequences
A person that can’t make enough insulin or whose body won’t recognize insulin will have very high blood sugar levels. Eventually it will lead to diabetes, requiring medication and/or insulin shots. Sometimes diabetes is caused by diet and obesity (Type 2), and this type can be reversed through diet changes and weight loss.
Prevention
Not all issues related to insulin production/resistance can be prevented. Often times it is an issue of genetics or an autoimmune disorder where the body attacks itself. It is always beneficial, though, to manage blood sugar levels by eating regular, nourishing meals, exercising regularly, and managing stress.
Cortisol
Cortisol is made in the adrenal glands that sit on top of the kidneys and is commonly known as a “stress hormone.” It has three main functions:
1. Stimulates sympathetic nervous system in fight-or-flight situations by activating anti-stress and anti-inflammatory pathways. Cortisol floods the body with glucose (sugar) and sends it to large muscle groups, allowing us to fight or run from the stressor.
2. Cortisol responds to low blood sugar levels in the early stages of fasting by liberating sugar from stores in the liver. However, during starvation or prolonged fasting, cortisol blocks insulin from storing sugar, allowing its immediate use in the blood. This causes insulin resistance.
3. Suppression of the parasympathetic nervous system, preventing the rest-and-digest function to happen in the body.
Long-term consequences
A person experiencing long-term stress will have a constant flow of cortisol pumping through their body. Too much cortisol is hard on your liver, pancreas, blood sugar and digestive tract. When a person has constant high blood sugar levels, it triggers the pancreas to make insulin. We just learned that cortisol blocks insulin, so the body becomes insulin resistant. Meanwhile, cells are starving for sugar, and send signals to the brain to eat more food. This causes overeating, and for a stressed-out person whose digestive tract (parasympathetic) is shut down, things can start to get pretty uncomfortable. It’s a vicious cycle.
Prevention
Stress management is the obvious cure to the harmful effects of too much cortisol. That will look different for each individual, but some ideas include: gentle exercise, regular and nourishing meals (every 4 to 5 hours), cognitive therapy, meditation, adequate rest, and so on. Exercise is a critical stress-manager, because it is the only mechanism that can bring blood sugar down without the use of insulin. That’s good news for someone with too much cortisol, blocking the insulin pathway!
Ghrelin
Ghrelin is made in the stomach and is commonly known as the “hunger” hormone. I remember it as the hormone that makes your tummy growl… ghrrrrrelin… When our stomach is empty, ghrelin is absorbed so it can send a message to our brain to feed us. When the stomach is stretched, it stops firing.
Long-term consequences
If a person chooses to restrict food through dieting, or in extreme cases of starvation, they are ignoring ghrelin’s “knock at the door.” What happens then? Cortisol kicks the door down and brings glucose from the liver store, triggering that whole stress-response process again.
Prevention
Keep reading for the leptin prevention, because these two hormones work hand-in-hand.
Leptin
Leptin is produced in fat tissues and is commonly known as the “satiety” hormone. Leptin inhibits ghrelin when the stomach is full; and ghrelin inhibits leptin when the stomach is empty, because they have the same receptors in the brain.
Long-term consequences
If a person chooses to ignore leptin’s fullness signals they will overeat. Now, if this is just an occasional thing around holidays and celebrations, your body will naturally re-boot itself and you will eat less at the next meal. However, when done consistently (think: constant bingeing) weight gain will ensue and frequent high blood sugar levels will cause all the problems discussed before with insulin.
Prevention
Prevention tactics for both ghrelin and leptin can be achieved through listening to and honoring your hunger and fullness. Principle Number 5 in “Intuitive Eating” is the best way I can help you with this. “Feel your fullness” as you are eating meals. Here’s a diagram that can help:
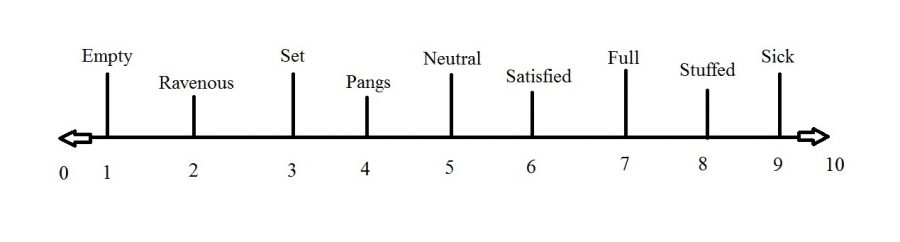
Take a time-out halfway through your meal and use this scale to assess your fullness. Are you at a 4? 5? Does the food still taste good? Is it satisfying you? If so, continue eating until you reach 6 or 7 where you are comfortable and satisfied. It is also important to remember that starting a meal at the 0 to 2 stage of hunger will inevitably cause you to overeat. Try to start most of your meals at the 3 or 4 level where it is easier to regulate your hunger and cravings.
The effects of sleep on hormones
Many convincing studies are showing that not getting enough sleep increases cortisol and ghrelin levels while decreasing leptin activity and insulin sensitivity. Thus, your brain thinks it needs energy from food when it actually needs energy from sleep!
What can I do to regulate my hormones?
Lets review. Here are the top 5 ways to regulate your hormones in relation to hunger and fullness:
1. Get adequate sleep.
2. Exercise in a enjoyable way—not too much, not too little.
3. Eat regular, nourishing meals made up of a variety of foods.
4. Manage your stress in healthy ways—social activities, hobbies, relaxation, meditation, cognitive therapy (if needed) and numbers 1-3 above.
5. Listen to and honor your hunger and fullness cues.
And there you have it! Who would have thought there was so much going on in your mind and body when you are eating (or not eating) food?
Featured Product
(Includes Affiliate Link)
Sources:
http://www.todaysdietitian.com/newarchives/111609p38.shtml
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065172/
Tribole, Evelyn, and Elyse Resch. Intuitive Eating: a Revolutionary Program That Works. St. Martin’s Griffin, 2012.