How a Type-1 Diabetic Cut His Insulin Use by HALF
Health Signs and Symptoms
Almost 10 years ago my 50-year-old father started experiencing some strange symptoms: unquenchable thirst, blurry vision, and unexplained weight loss. He was hardly getting any sleep at night, because just as fast as he could drink any fluids they were all coming back out of his system. After explaining this all to me, I suggested he see a doctor right away. Blood tests revealed his post-prandial (after meal) blood glucose levels at 506 mg/dl. Normal levels should be under 140 mg/dl.
Diagnosis
After all the tests came back, it was determined that Dad had Type-2 Diabetes, a metabolic disorder most often caused by obesity. It was thought that his body developed a resistance to insulin, the hormone in our bodies responsible for transporting glucose from blood and into cells. This was shocking to me. My dad had been thin ever since I could remember, and his buddies gave him the nick name, “String Bean.” He was always a very active person—working a hard labor job, coaching sport’s teams, or refereeing games on the weekends. How could he develop a disorder related to obesity?
It took three weeks of diet, exercise, and metformin to get his blood glucose under 200 mg/dl. Metformin is a drug which helps the body lower blood glucose levels by increasing sensitivity to insulin. It also decreases the amount of sugar produced by the liver, and it slows the absorption of sugars from the intestines into the bloodstream after meals. After time, half of a pill was not enough. Soon he was taking as many as TWO pills of metformin and his blood sugar numbers shot up to the 300’s again. Dad was wasting away, and at 130 pounds he weighed almost the same as me! He was following the counsel of his dietitian by regulating his carbohydrate intake, exercising regularly, and pricking his fingers to measure his blood glucose several times a day. It was all to no avail. At this point, his doctor realized there had been a misdiagnosis. Three-and-a-half years after his first diagnosis, it was determined that he had Type-1 Diabetes–not Type 2.
Causes
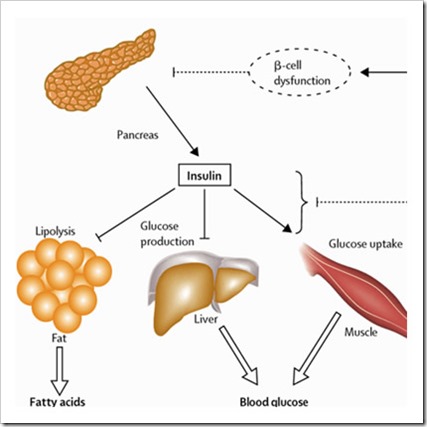
Type-1 Diabetes is an autoimmune disorder where the Beta cells (β-cell) in the pancreas, responsible for making insulin, are destroyed. Dad could have taken a whole bottle of Metformin and it would have done nothing for him, because there was no insulin for the medicine to stimulate! Type-1 is referred to as “Juvenile Onset” diabetes because most patients are diagnosed before the age of 30. Dad is a rare exception to this rule. Science still doesn’t know what exactly causes the onset of the disease, but we do know that nothing can prevent Type 1 Diabletes from occuring.
Photo Credit: http://www.news-medical.net/health/What-is-Insulin.aspx
Treatment
Treatment for Type-1 Diabetes has three parts: Insulin administration, Diet, and Exercise. Dad received lots of instruction about how to administer the exogenous insulin. After each meal or snack, he pricked his fingers to test his blood sugar. That determined how many units of insulin he had to give himself via a syringe taken in the belly or thigh. Dad also met with a dietitian who taught him how to manage carbohydrate intake. What he got out of that instruction was that meat, eggs, and cheese were carbohydrate-free and could be eaten in any quantity, but grains, fruits and sweets should be restricted. He often had to take a rigorous jog or bike ride at night in addition to his active-labor day job in order to get his glucose to go back down after dinner.
As time went on, Dad’s energy waned, he started gaining weight and was taking more and more insulin to manage his high blood glucose levels. A typical diet for him included 8-10 servings of animal products per day which included free-range venison, poultry, yogurt and cheese. He constantly snacked on nuts. All carbohydrates, including whole grains were self-restricted, and he was careful not to over-do starchy vegetables like potatoes and corn. However, his sweet tooth often overcame his efforts to restrict carbs and he often snitched at sweets lying around the house or break room. In order to manage healthy blood glucose levels, he was taking 10-12 units of insulin after every meal. Finally, he came to me asking for help losing 10 pounds. Here is what I told him about his diet and how he could make a few simple changes:
Grains: Stop worrying so much about every “starchy” food you eat! Instead, focus on how whole your grain choices are: Get a really good loaf of 100% whole wheat bread. Try quinoa, barley, and brown rice in soups, salads, casseroles and dishes.
Fruits: Aim for fresh fruits instead of canned or dry. Add chopped apples, strawberries, bananas or peaches to your morning oatmeal. Include it in salads.
Vegetables: DOUBLE your intake. Instead of 3 servings a day, aim for 6! This may sound crazy, but loading your plate with lots of vegetables means getting all of the vitamins and minerals your body needs in order to manage bodily functions.
Meats: SWAP your meat portions with your vegetable portions. Instead of a 9-ounce steak with a side salad, have a full salad with a few slices of steak on top. Instead of four scrambled eggs with a sprinkling of veggies mixed in, cook up a load of veggies and add just one egg mixed in. These Hearty Vegetable Ranch Eggs became a favorite for Dad.
Beans/Legumes: Although beans are often labeled as starchy, they also have TONS of fiber in them. They won’t spike your sugar like a starchy piece of bread does because the extra fiber helps slow the digestion in your gut. Try beans in your salads, soups, casseroles and even eggs!
Nuts: Although nuts are carbohydrate-free and a great source of fiber, there is still 1 gram of fat in every nut you eat. A reasonable serving of nuts each day is 1/4 to 1/2 cup each day, rather than 2 full cups each day.
Cheese: Another carb-free food, cheese is a great source of calcium, and it is also high in fat. This does not mean you can’t eat cheese any more. An amount closer to 2 or 3 ounces rather than 5 or 6 ounces each day should be the goal.
Added Fat: Some ways to include healthy fats in your diet are to mash avocadoes for topping salads, or make homemade dressings with more vinegar and less oil than store-bought dressings.
Here is the thing with all meat and animal products: they cause inflammation! I don’t care how this relates to weight loss, but I do care what it means for diabetics and their insulin intake. Inflammation puts the body in a state of stress. The body reacts to stress by releasing glucose into the bloodstream. For diabetics, this means taking even more insulin to manage blood glucose levels. The cure for this is quite simple: eating a plant-based diet by decreasing animal products and increasing antioxidant intake through vegetables and fruit will repair inflammation and allow the body to take up insulin better.
Outcomes
After about two to three months of eating a more plant-based diet, Dad lost his goal of 10 pounds. More impressive was that he now needed just 3-4 units of insulin after each meal! He decreased his insulin intake by more than half of what he needed before! He no longer needed to exercise excessively in order to get his blood sugar down at night and he had TONS of energy! Dad’s diet now consists of about 3-4 servings of animal products daily instead of the 8-10 servings he previously consumed. He found that fruit and beans didn’t effect his insulin like he thought they would and he could eat 2 or 3 servings of each. The icing on top of all these positive results is Dad’s vision got better! He went to the doctor and got a weaker prescription for glasses because once all the excess sugar flushed out of his system, his blurry vision left too. Success!




This is a very clever theory about the cause of your dad’s diabetes and I’m impressed that you have done the research and you can appreciate how hepatic glycogen conversion can affect blood sugar (sometimes in surprising ways). Not many people know this about the liver.
And I’m so sorry your dad went so long with the wrong diagnosis. Based on what you’ve written about your dad’s experience, I suspect your dad has type 1.5 LADA (latent autoimmune diabetes in adults). There is no medical diagnosis code for type 1.5, so many people with type 1.5 get misdiagnosed with type 2.
Type 1.5 eventually turns into full-blown type 1. With type 1.5, your insulin-producing beta cells get killed off, but they get killed off slowly (over months or years). This prolonged murder of beta cells is called the “honeymoon” period, during which your pancreas just produces less and less insulin as your blood sugar, in turn, goes higher and higher. All type 1s have a honeymoon period. With kids, it’s a LOT shorter (months). In adults with type 1.5, this honeymoon period can last years.
Your dad did not cause or accelerate his diabetes diagnosis with his eating habits. To be clear, type 2 diabetics don’t cause their diabetes, either, but type 2s can *accelerate* their diabetes onset with eating habits (note the nuance here). This is not true with type 1s.
The GAD autoantibodies that attack the insulin-producing beta cells work independently and don’t react to pancreatic overload. You dad could have been on a keto diet for his entire life and he *still* would have become diabetic because the GAD autoantibodies would have killed his pancreatic beta cells anyway.
I do think that the metformin initially did help him during the time his pancreatic beta cells were dying their prolonged death. Type 1s have had a lot of success taking metformin, even though it’s indicated for type 2s. And, based on your dad’s insulin dosing (even the dosing he was on prior to the new way of eating), it doesn’t look like he has insulin resistance. The pancreas wasn’t working overtime. It was slowly being crushed by GAD autoantibodies, and there isn’t a darn thing he could have done about it. If they’d done a C-peptide test and a GAD autoantibody test, they would have diagnosed him correctly at the initial onset.
I could write more, but your blog sidebar is making me hungry, so I’m going to go recipe hunting on your website now. 🙂
Thanks,
Kara
Kara,
Thank you for taking the time to comment. I’m not an expert on diabetes, so I appreciate your insight on what may have caused the insulin dependency. If what you are suggesting really is the case for my Dad, I sure hope that it isn’t genetic–or at least that I will somehow not inherit that gene. 😉 One thing that’s for sure is Dad is feeling better than ever thanks to more complete nutrition. Enjoy recipe hunting!
Over the years, things changed… dx’d at age 8, she is now almost 20. Breakfast has always been difficult due to the Dawn phenomenon. Puberty? Let’s not even mention it. 👿 Lower GI foods, balanced with protein, fat and fiber help with spiking after meals. Prebolusing was very important when she was younger…now that she does it all herself (living away at college) she doesn’t do what I would like. Lol. No matter the type, diabetes is a beast.
I’m not a doc or nutritional expert, but I’m the mom of a type 1diabetic. Type 1 is an autoimmune disease, in which the pancreatic beta cells (which produce insulin) are attacked by the patient’s own immune system. Type 2 patients can become insulin dependent over time, but Type 2 is a metabolic disorder, not autoimmune. Just a factoid or two 😁 I’m glad your dad is doing well now.
Thanks for the input! I think mothers of diabetics know about as much as the experts. Have you found any special dietary practices that work well for your child?